INTRODUCTION
Injuries happen on the sports field and while we can potentially reduce the risk, they will always occur. However, the number one priority for all S&C coaches in my opinion is to ensure their athletes do not get injured in the weight room. Injuring athletes with general training (i.e. resistance training) is something we have a huge control over and therefore, we are in a position to significantly prevent.
Seeing as the shoulder complex is one of the most injured regions with resistance training1, there are a number of things we can do to ensure our athletes stay healthy in the gym. Here are 5 things coaches should ensure their athletes do that I believe have the potential to significantly reduce injury risk at the shoulder complex for athletes.
- Make sure an athlete can pass the Bilateral Shoulder Elevation Test
I value bilateral shoulder elevation test (BSET) massively as a basic screen in order to understand how an athlete moves at the shoulder and spine. In fact, I wrote a whole article about it for SCJ.2
If an athlete can’t get their arms above their head without using compensations, they have no business doing overhead lifting. This is not only applicable for pressing movements. If an athlete can’t get their hands above their head, what do you think the bottom position of their chin up will look like? The likelihood is there will be significant stress placed on a number of structures to make up for the loss of motion. And under high loads (such as what is seen in the chin up) this could be seriously problematic.
This may even result in excessive loading being placed on structures far from the shoulders. If an athlete lacks shoulder elevation and they need to get their hands above their head to finish their Press, it’s not uncommon to see them go straight to a spinal extension pattern to get the rep. Do this enough times and it could cause problems in the future.
So making sure the athlete can get into good positions before you load these patterns will go a long way in ensuring they preserve the health of not only their shoulder complex, but also the neighbouring segments such as the lumbar spine.
Figure 1 shows how to perform the BSET. The findings can be interpreted using the model in Figure 2.
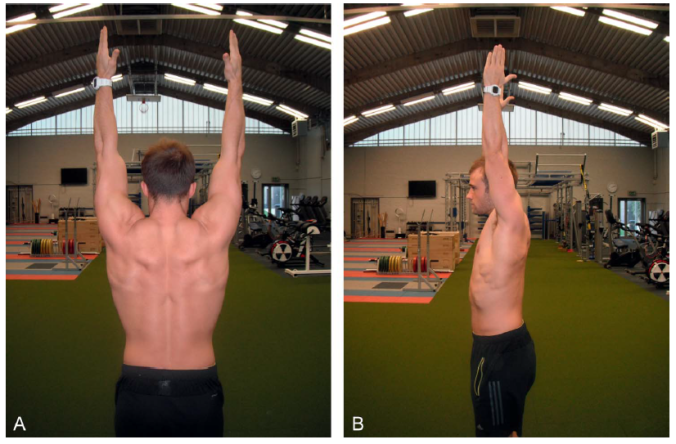
Figure 1. The BSET is performed with the athlete reaching above their head with extended elbows. The arms should move in the scapula plane and at the top position, the coach should determine if the athlete has used the thoracic spine, scapulothoracic articulation and glenohumeral joint sufficiently to achieve this position.
- Chase mobility… If the athlete doesn’t already have it
Because the scapula and therefore the humerus reside on the thoracic spine, I always teach students that the thoracic spine is like the foundation for the house to be built upon (the house being the scapula and the humerus in this analogy). Wherever the thoracic spine goes, the scapula goes and that directly impacts what happens at the glenohumeral joint.
A mobile thoracic spine is crucial in order to get the scapula into a good place. Extending the thoracic spine facilitates upward and posterior rotation of the scapula. These movements are important for shoulder health as they move the acromion further from the humeral head, decompressing the subacromial tissue. So from this standpoint, poor thoracic spine mobility may be associated with the onset of external shoulder impingement in athletes who lift above head. You can read more about this in a previous blog post I have on here.
This is exactly the same for the scapula downward rotators. The pectoralis minor, levator scapulae and rhomboids will prevent the scapula from achieving the 50-60˚ of upwards rotation it likely needs to in order to support glenohumeral function.
And it is no different with the muscles that limit glenohumeral joint elevation. A tight pectoralis major, latissimus dorsi or teres major will all cause a failed BSET.
Importantly, once the BSET has been performed by an athlete, the coach can use the findings to get some idea as to what muscles/joints might be limiting the movement. Likewise, the BSET can be used to identify what muscles aren’t functioning optimally in elevating the shoulder (see Figure 2).

Figure 2. Process for identifying a potential restriction during the BSET. ST = Scapulothoracic, GH = Glenohumeral
These findings can be confirmed through isolated testing. My article Shoulder Function During Overhead Lifting Tasks: Implications for Screening Athletes in the NSCA’s SCJ shows all the relevant tests that may be employed by the S&C coach to identify mobility restrictions. This article can be found here:
https://www.nsca.com/education/articles/shoulder-function-during-overhead-lifts/
So if the athlete doesn’t have sufficient mobility, then get the mobilisations/stretches in the programme. When deciding how to prescribe mobility/flexibility work, have the athlete do the isolated test for a baseline score, then implement an intervention (as shown in Figure X) and see if it changes their baseline. If it doesn’t, try something else.
- Train the scapula upward rotators
The scapula upward rotators are hugely important for the health of the glenohumeral joint. I’ve already spoken about why scapula upwards rotation is important for preventing external impingement, but upwards rotation is also important for maintaining the length-tension relationship of the rotator cuff muscles. A scapula that doesn’t sufficiently upwardly rotate usually results in a larger amplitude of movement at the glenohumeral joint leading to greater lengthening of some of the cuff muscles, causing a reduced overlap of its actin and myosin filaments.
The muscles that upwardly rotate the scapula are the trapezius (predominantly the upper and lower fibres) and the serratus anterior. Each one of these muscles are tremendously important for the function of the shoulder and should be trained in most athletes. Here are a few example exercises to strengthen these muscles.
- Upper trapezius: Snatch grip shrugs and overhead shrugs – basically shrugging with shoulder abducted beyond 30˚ as this is required for the upper trap to elevate the scapula.
- Lower trapezius: Prone V’s and band W’s.
- Serratus anterior: Any crawling movement done in prone and loaded push ups (ensuring scapula protraction at the top).
- Train the rotator cuff muscles
This has been a controversial topic in the past, with some practitioners suggesting that isolated rotator cuff training is useless and doesn’t reduce injury risk. I don’t buy that at all as there is some good evidence to suggest that weak external rotators increases the risk of incurring a shoulder injury.3
Facilitating a muscle imbalance through poor programming is a great way to disrupt the arthrokinematics of a joint and degrade tissue. When we consider the functional role of the rotator cuff muscles is to centrate the Glenohumeral joint, it’s not hard to see that if they are weak relative to the pectoralis major (as an example), shoulder health may become compromised. Therefore, if your athlete can BB bench press 165kg for 1 rep but can only do a side lying DB external rotation with 4kg for 10, it is unlikely to work out well for the athlete in the long run.
In my own practice as a coach, I use the athlete’s bench press to guide where their rotator cuff strength should be. As the bench press involves a high level of strength from the pectoralis major, anterior deltoid and latissimus dorsi, comparing this lift to rotator cuff strength can inform the coach as to the relative strength of the athlete’s stabilisers. I like to see athletes be able to do rotator cuff work with approximately 8-10% of their 1RM Bench Press for 8-10 reps. So if a guy has a 120kg Bench, I think he should be able to do side lying DB external rotations with approximately 9-12kg dumbbell for 8-10 reps. I use the approach with some of the scapula work I spoke about previously.
I’ll be the first one to say that I’m not aware of much research to support this ratio. I also think a number of variables play into the level of appropriateness of this ratio. As an example, if a powerlifter can Bench Press 250kg, do I think they should be able to do rotator cuff work for reps with a 25kg dumbbell? Probably not. But if that athlete can only do 4kg for 8 reps, I think it may be a problem.
Although I appreciate there are holes in this concept, I believe it’s built on a robust theoretic model. It’s something I have used a lot with good success in the athletes I’ve worked with. At the very least, this concept can be used with athletes to motivate them to strengthen some key shoulder stabiliser muscles.
- Monitor ALL overhead lifting
This is a trap I’ve fallen into before with athletes. I’ll calculate the exposure to traditional overhead lifting (e.g. chin ups, press, snatch, etc.), but won’t factor in exercises such as abs rollout. Even stuff like wall angels. Then, all of a sudden, my athletes are doing tons of high load overhead work that I’m not considering as volume that may be problematic (note: a wall angel can be high load if you aren’t very mobile. In order to overcome the stiffness of the tight muscles, high level contractions of the shoulder musculature are needed, therefore exposing the shoulder complex to high loads).
This is a major issue as exposure is primary risk factor for virtually all injuries (if you never run, you’re unlikely to tear the long head of the biceps femoris). In this sense, if we don’t manage exposure, then we aren’t controlling a primary risk factor to shoulder injuries.
I would also add other exercises that directly loads the glenohumeral joint into this calculation. If you prescribe upright rows, you should consider the volume allocated to this exercise. Same with lat raises. In fact, any exercises performed with the shoulder elevated above the 60˚ associated with the painful arc is of interest.
Once you know the volume that the shoulder complex is being exposed to, you can programme accordingly to ensure huge spikes in overhead lifting volume don’t occur in the weight room.
SUMMARY
Hopefully this post has given some coaches some ideas for programming for the shoulder complex. For the most part, each variable discussed is relatively obvious, but its surprising how many times these things fall out of an athletes programme.
REFERENCES
- Kolber, M.J., Beekhuizen, K.S., Cheng, M.S.S. and Hellman, M.A., 2010. Shoulder injuries attributed to resistance training: a brief review. The Journal of Strength & Conditioning Research, 24(6), pp.1696-1704.
- Howe, L.P. and Blagrove, R.C., 2015. Shoulder Function During Overhead Lifting Tasks: Implications for Screening Athletes. Strength & Conditioning Journal, 37(5), pp.84-96.
- Clarsen, B., Bahr, R., Andersson, S.H., Munk, R. and Myklebust, G., 2014. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. British journal of sports medicine, pp.bjsports-2014.








